Therefore, when we understand the pathogenesis of the clubfoot, the causes of the relapse will become clear.
TERMS
Relapse is one of the worst scenario for every clubfoot parent. It brings the worst thoughts about the condition itself and the treatment. Surprisingly though, when parents are asked to define a relapse, they are not fully able to name their thoughts and concerns. No wonder, even the doctors find it difficult to define what a relapse is?
For some of the physicians and clinicians a relapse means a complete return to the abnormal foot position, and for other specialists it means a return of at least one of CLUBFOOT COMPONENTS. As one can see, it is not that obvious – the multiple options are like unsolved puzzles or scattered bricks where nothing seems to fit together.
Dr. Ignacio Ponseti and Dr. Jose Morcuende defined a relapse as a return of two of the essential clubfoot components: equine position of the calcaneus and heel varus.
VARIATIONS
Clubfoot defect components can return in different variations meaning to different degrees or in various clubfoot parts.
Relapses affecting the forefoot or middfoot occur significantly less than relapses of the hindfoot but these second ones are more important and more difficult to correct as it requires more knowledge, experience, involvement and patience.
Relapse of forefoot adduction (metatarsus adductus) to less than 20° was observed by Dr. Ponseti in less than 1/4 cases. Forefoot correction is rather permanent, easy to achieve by applying 2-3 casts when the relapse occurs. Dr. Ponseti also admitted he noticed a persistent relapse of forefoot adduction only in two cases, however they had been previously treated by Lisfranc joint capsulotomy, which resulted in stiffness and pain in adulthood.
Relapse of cavus is usually soft and responds well to manipulation and casting as long as the pressure during correction is directed upwards – to the first metatarsal bone. Percutaneous plantar fasciotomy is rarely required – only in ca 6% of cases. If there is a need to correct a burdensome plantar flexion of the first metatarsal bone, a transfer of the long toe extensor muscle to the first metatarsal bone can be performed.
CAUSES

In children with clubfoot, FOOT ANOMALIES are large and significant with a strong tendency to relapse irrespective of the treatment method. It is mainly related to the multi-faceted nature of the deformity. As Dr. Ponseti explains ”Once we understand clubfoot pathogenesis, the causes of relapse will be clear” – in part the causes of relapse are understood. Claiming that a relapse occurs because the foot was not fully corrected is unwarranted.
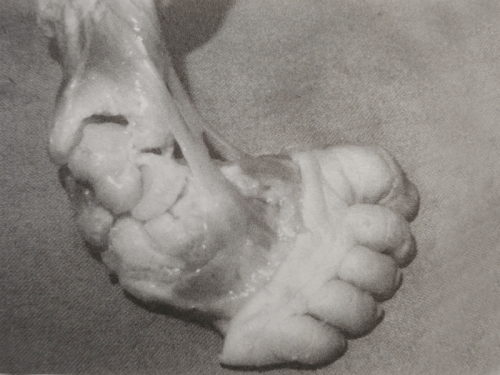
Soft tissues have a “deforming power”, meaning there are certain pathologies that are active for a long time, pulling the foot into a wrong position. The tendons, ligaments and muscles on the midfoot side are shorter and stronger comparing to those on the exterior side. A slight decrease in a muscles size is also noticeable together with an excess collagen synthesis with a fibrosis withdrawal in medial and posterior tarsal ligaments, in deep fascia, Achilles tendon and posterior tibial muscle. The fibrosis affects calf triceps and other foot ligaments and tendons. All of these deformities result in a severe equinus (foot pointing down), relocation of navicular bone, heel varus and adduction which are all CLUBFOOT CHARACTERISTICS.
RISK GROUPS
Does the relapse risk affect each congenital clubfoot child? Yes, it does. Each clubfoot child is at risk of a relapse! Relapse tendencies start being active during second pregnancy trimester, as this is the time when clubfoot deformity forms, and is most active till a child is 4-5 years old. This is mainly caused by an increase of collagen in tendons and ligaments of mammals, most likely also of human. Besides, the speed of foot growth increases after child’s first year, and increases significantly after the age of five.
It is wrong to believe that children whose clubfeet were categorised as difficult or resistant to treatment, as well as those whose clubfoot deformities were classified higher (according to Dimeglio or Pirani score) will for sure face a relapse, whereas those with softer will not. The severity of deformity assessed after the birth is not a reliable indicator defining a possibility of a relapse in the future. It is true, however, that there are some risk groups, where a relapse can be determined as of higher or lower probability.
LOW RISK
- children with very loose ligaments (large amount of collagen)
- children with less severe deformities
- children with POSITIONAL CLUBFOOT have no relapse
- children over 5 years old
- children using the brace according to the protocol till they are 4-5 years old
- children with no sudden growth spurt
HIGH RISK
- premature babies
- children with hard, stiff clubfeet and thin calves
- children with higher degree of deformity
- ATYPICAL OR COMPLEX CLUBFOOT, neurological or syndromic
- children after foot surgery, regardless of age
- children up to 2 years of age
- children using the brace inconsistent with the protocol for less than 4 years
- intensive growth periods in children with less activity at the same time
SIGNS OF THE RELAPSE
At the very beginning a relapsed clubfoot is flexible. Some dynamic deformities start to occur e.g. during running, walking or standing. If they are not noticed at the right time, they can transform into static deformations, which become permanent and the foot begins to stiffen loosing correction even more.
Most relapses evolve gradually and are difficult to recognise at early stage, as the changes are noticeable once a child starts to stand and walk alone


DECREASES
ON TIP TOES
STIFFNESS
LATERAL SIDE
TURNS INWARD
INTOLERANCE
IS THIS A RELAPSE?
When toddlers learn to stand and walk, they often bear weight on their feet by twisting them in all possible directions. Parents tend to worry and think this may be a relapse whenever child’s foot is in a strange position. But it is not the case. It is recommended to check if the foot is flexible, can be manipulated in each direction and whether it returns to its normal position. If yes, there is no need to panic and most likely your child is simply learning how to balance its body by putting weight on its feet, which are at that time weak and still haven’t learnt their functions.
IF YOU HAVE ANY DOUBTS ABOUT YOUR CHILD’S FEET AND THEIR FUNCTIONS
– CONTACT AN EXPERIENCED DOCTOR PROMPTLY!
CRUCIAL ELEMENT
Relapse often occurs when a child is at the bracing stage.
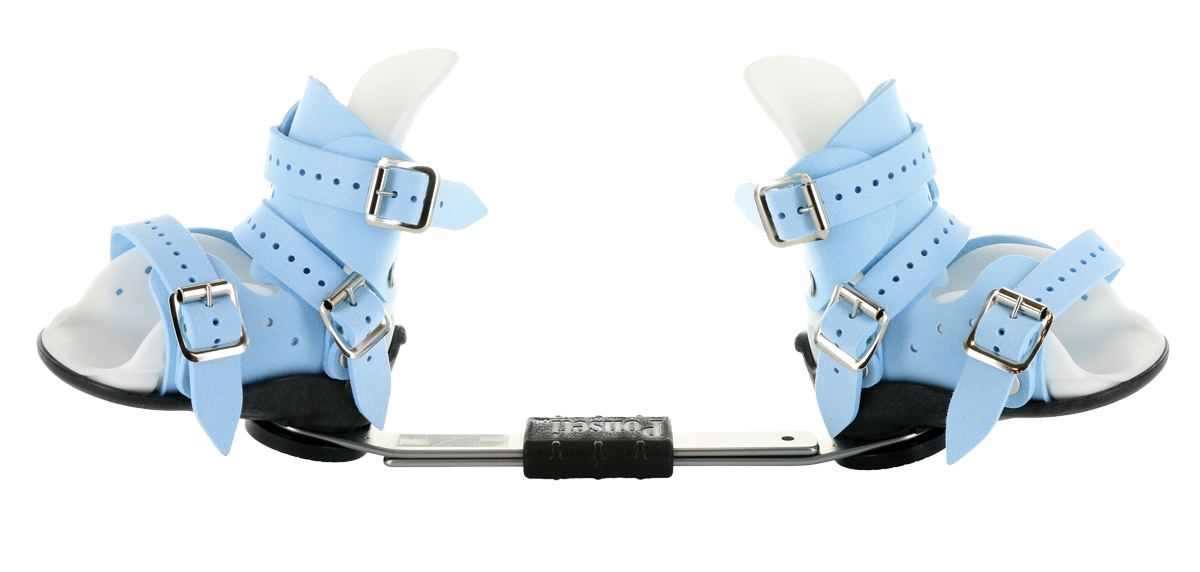
FOOT ABDUCTION BRACE is to maintain the correction resulting from previous treatments – casting and Achilles tenotomy. Any brace modifications related to its structure, time and way of wearing usually result in a very quick return to foot incorrect position.
WATCH OUT!
TREATMENT BY PONSETI METHOD IS VERY FAST. IT TAKES 4-6 WEEKS TO FULLY CORRECT THE FEET,
THEY BEGIN TO LOOK NORMAL AND ARE FULLY FUNCTIONAL.
THIS IS HOWEVER A TRAP, BOTH FOR PARENTS AND DOCTORS!
DESPITE QUICK AND NOTICEABLE TREATMENT EFFECTS AND AN ILLUSION THAT FEET
ARE NORMAL, HEALTHY AND LOOK CORRECT,
CHILDREN STILL NEED TO “FIGHT” FOR MAINTAINING THE CORRECTION.
THE MAIN CAUSE OF A RELAPSE IS NOT USING OR WRONG USAGE OF THE FOOT-ABDUCTION BRACE.
THIS IS THE KEY TO SUCCESSFUL TREATMENT.
BRACE SHOULD BE WORN AT LEAST UNTIL THE AGE OF FOUR.
YOUR PARENTAL GUIDANCE IS FUNDAMENTAL AT THIS PHASE OF TREATMENT
AND IT DEPENDS ON YOU WHETHER YOUR CHILD WILL HAVE FULLY FUNCTIONAL AND FLEXIBLE FEET!
WHY IS THE BRACE NECESSARY?
EXTERNAL ROTATION
GOOD ADJUSTING
FOOT ABDUCTION BRACE needs to be properly selected, adjusted and applied.
NO FOR ORTHOSIS!
HOW LONG?
IF A RELAPSE HAPPENS…
In the first 20 years of Ponseti practice relapses happened in about half of his patients at the age from 10 months to 5 years (on average 2,5 year). Ponseti noticed that a relapse occurred between two to four months from the moment when parents decided to give up wearing a brace because feet “look good” and because the correction seem stable to them. With the evolution of his method and by making some amendments to the treatment as well as by increased Internet influence, Ponseti noted that:
I have further overcorrected the deformity in the last plaster cast, to be certain that the calcaneus is fully abducted and its anterior joint surface is well under the head of the talus. Secondly, there has been greater awareness on the part of the parents regarding the importance of maintaining the night splints after correction for three to four years.
Treatment way depends on child’s age, type of relapse and its severity. The method will look different for 8-month-old children, for 3-year-old and for 6-year-old kids. Regardless of age, the treatment should start with re-casting and not an invasive surgery without attempts to re-correct the feet by using simple and at the same time effective ways.
At first, forefoot adduction, heel varus and cavus deformity is corrected, exactly like in a standard PONSETI METHOD. Equinus position of the heel can be corrected after other components are fine. Otherwise, number of additional deformations can occur (e.g. rocker bottom foot), increasing of cavus or over-correction of foot in Chopart joint or the clubfoot is not corrected.
CASTING
The first part of relapse treatment method is re-casting. It gives good results without using invasive methods.
In general, the correction can be regained in four to six weeks by manipulations and casts.
Depending on child’s age and the severity of relapse the cast may be long-leg cast (from toes to groin, with the knee bent at an angle of 70-90°) or short cast (under knee). The casts are changed weekly or every two weeks. The cast should be abducted significantly and at maximum dorsiflexion in the ankle joint.
You can read about the features of a good cast on TREATMENT BY PONSETI METHOD.
LONG-LEG CAST
most often used when the foot is no longer at its correct position and it is necessary to do a re-correction, in order to release calcaneus from its wrong position. This kind of a cast prevents rotation of the ankle and talus. As the foot needs to be positioned under talus in abduction, the talus can’t rotate.
TENOTOMY
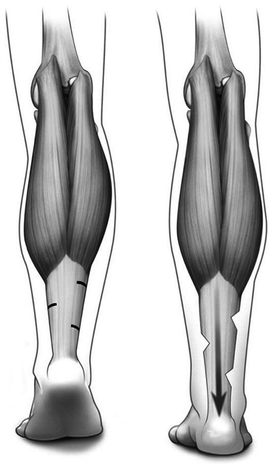
Percutaneous Achilles tenotomy may need to be repeated when dorsiflexion is less than 15°. However there are limitations as to the child age.
Dr Ponseti believed that the best time for doing this surgery is until a child is one year old. There are though some physicians who perform this surgery when children are much older. Commonly used solution, when a child is older (over 2,5 years old) is to perform other type of tenotomy, also percutaneous (without the need to open the back of the foot surgically). This procedure is called Hoke tenotomy, which is percutaneous, triple hemisection of Achilles tendon. It gives better results than other tenotomies for older children. There are no tendon scarring at the point of elongation. The tendon is also not exposed to injuries in this place. Posterior capsulotomy is rarely required.
FAB
As mentioned before, THE BRACE should be used after the treatment and after re-treatment. It maintains the foot in the correct position. If the brace is not used , a relapse may occur. Treatment takes much time, is expensive and stressful.
If a child is at the age where the use of brace may result in high intolerance or even risk of not using it, there is a possibility to use ADM (ABDUCTION DORSIFLEXION MECHANISM). However, it is a doctor who decides about its parameters as it is necessary to choose the appropriate spring force.
SURGERIES
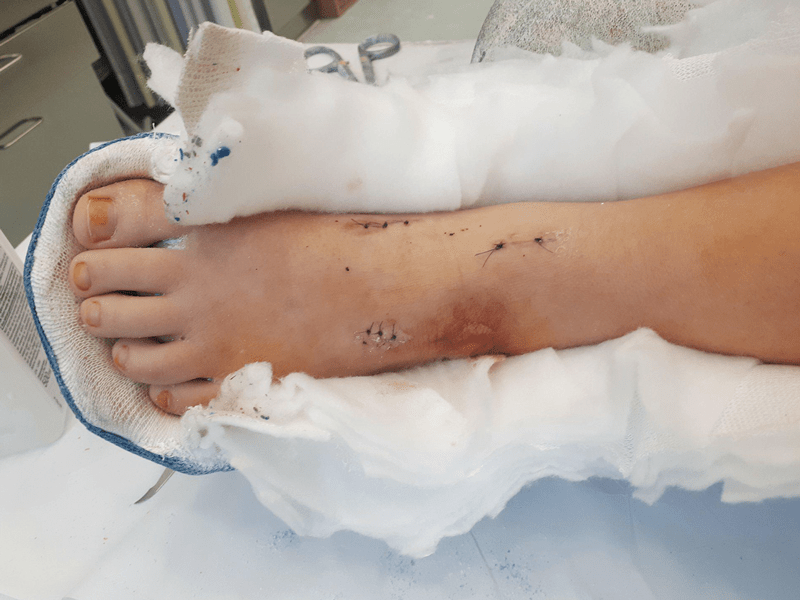
When there is a strong imbalance in the clubfoot caused by tendons and ligaments pulling strongly from the medial side of the foot, which results in foot supination and heel varus ( the child begins to walk on the lateral side of foot, rotating the foot inwards), the first surgery to be applied in Ponseti method (described by the author himself) is the transfer of tendon of the tibialis anterior muscle to the third cuneiform bone (ATTT – Anterior Tibialis Tendon Transfer).
ANTERIOR TIBIALIS TENDON TRANSFER
The anterior tibialis tendon should be transferred in a way as not to lose its eversion power. In the case of a wrong transfer, the foot will not SUPINATE at all affecting the correctness of walking. The tendon should not be transferred to the fifth metatarsal or to the cuboid, as this would excessively evert the foot, causing severe foot pronation and heel valgus.
The foot after ATTT is flexible and functional almost immediately after removing post-operative casts. In a very short time children are back to full activities without the need for rehabilitation. There are no extensive scars on the foot, which are not only unaesthetic but also can cause further relapses as the scar is not elastic and pulls the foot into wrong position. The only marks after the surgery are three small incisions on the skin, through which the entire surgery takes place. Some consider it to be “orthopedic laparoscopy” because there is no need to open the body to see all the structures within the foot.

Other types of surgery may or may not be necessary but they should never be the first solution in the treatment of congenital clubfoot relapse in children. Due to re-casting and simple but effective procedures, it may turn out that invasive surgery is completely unnecessary. Unfortunately, doctors around the world prefer surgery because it is an easier solution then weekly cast change for many reasons e.g. time and cost-effectiveness . Besides, the improvement of the foot shape is visible immediately but it is apparent as all invasive surgeries have so called ‘secret enemy’ – the need to repeat them. Every serious intervention in the foot structure strains its functionality and weakens it. Most often adults who were treated with surgery (without Ponseti method) complain of pain, stiffness, and difficulties in everyday life.
CLUBFOOT TREATMENT SHOULD NEVER START WITH AN INVASIVE SURGERY!
CLUBFOOT RELAPSE TREATMENT SHOULD NEVER START WITH AN INVASIVE SURGERY!
STATISTICS
All the statistics regarding relapses cannot be grouped together. The difference between the collected data is often very significant. But they do have one common factor: relapse depends on the use of the brace and it is the crucial element that has great influence on the recurrence.
As many as 78% of relapses are connected to the no wearing the brace according to the Ponseti protocol, whereas only 7% of relapses concern children who used the brace according to the protocol. Common reason why parents decide not to continue wearing the brace is the false belief that the foot is fine. Other reasons are: parents education, social status, defect awareness, understanding of brace usage and it’s importance.
Research often shows the necessity for better understanding of Ponseti treatment method by those who apply it, also the need for applying it correctly. Data regarding the EFFECTIVENESS OF THE PONSETI METHOD in some centres may reach the level of 26,2% which in comparison to dedicated centres, where the effectiveness is 98-100% – is shocking and devastating. This proves that Ponseti treatment method may not be used identically by physicians and healthcare staff. Without any doubts it is the field one should focus on – better understanding of treatment method and of its correct application, increasing parents awareness in the field of brace usage as a prevention from relapse.
Statistics presented below , elaborated by DR. JOSE MORCUENDE from PONSETI INTERNATIONAL ASSOCIATION, show how important it is to wear a brace as a method of relapse prevention:
1 year old
-
- 90% of children had a relapse in their 1. year of life when the brace-wearing has been discontinued,
- 70-80% of children had a relapse in their 2. year of life when the brace-wearing has been discontinued,
- 30-40% of children had a relapse in their 3. year of life when the brace-wearing has been discontinued,
- 10-15% of children had a relapse in their 4. year of life when the brace-wearing has been discontinued,
- 6% of children had a relapse over 4. year of life when the brace-wearing has been discontinued.
over 4th year of life
IF YOU THINK YOUR CHILD MAY HAVE A RELAPSE –
– CONTACT AN EXPERIENCED DOCTOR IMMEDIATELY!!
THE LONGER YOU WAIT, THE WORSE THE DEFORMITY WILL BECOME.
SOURCES
RESEARCHES & STUDIES:
1. Ponseti I.V., Smoley E.N.: “The Classic: Congenital Club Foot: The Results of Treatment”
2. Ponseti I.V.: “Congenital Clubfoot. Fundamentals of treatment” (2nd edition)
3. Ponseti I.V.: “Relapsing Clubfoot: Causes, Prevention, and Treatment”.
4. Bhaskar A., Patn P.: “Classification of relapse pattern in clubfoot treated with Ponseti technique.”
5. Dobbs M.B., Rudzki J.R. et al.: “Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet.”
6. Halanski M.A., Maples D.L. et al.: “Separating the chicken from the egg: an attempt to discern between clubfoot recurrences and incomplete corrections.”
7. Mahan S.T, Spencer S.A. et al.: “Clubfoot relapse: does presentation differ based on age at initial relapse?”
8. Radler C.: “Kindlicher Klumpfuß. Rezidivbehandlung.”
9. Zhao D., Li H. et al.: “Prognosticating Factors of Relapse in Clubfoot Management by Ponseti Method.”
10. Zhao D., Li H. et al.: “Results of clubfoot management using the Ponseti method: do the details matter? A systematic review.”
11. Chu A., Lehman W.B.: “Persistent clubfoot deformity following treatment by the Ponseti method.”
12. Lourenço A.F., Morcuende J.A.: “Correction of neglected idiopathic club foot by the Ponseti method.”
13. Janicki J.A., Wright J.G. et al.: “A comparison of ankle foot orthoses with foot abduction orthoses to prevent recurrence following correction of idiopathic clubfoot by the Ponseti method.”
14. Ramírez N., Flynn J.M. et al.: “Orthosis noncompliance after the Ponseti method for the treatment of idiopathic clubfeet: a relevant problem that needs reevaluation.”
15. Zhao D., Liu J. et al.: “Relapse of Clubfoot after Treatment with the Ponseti Method and the Function of the Foot Abduction Orthosis.”
16. Scher D.M., Feldman D.S. et al.: “Predicting the need for tenotomy in the Ponseti method for correction of clubfeet.”
17. Thacker M.M., Scher D.M. et al.: “Use of the foot abduction orthosis following Ponseti casts: is it essential?”
18. Zionts L.E., Dietz F.R.: “Bracing following correction of idiopathic clubfoot using the Ponseti method.”
19. George H.L., Unnikrishnan P.N. et al.: “Unilateral foot abduction orthosis: is it a substitute for Denis Browne boots following Ponseti technique?”
20. Herzenberg J.E., Radler C. et al.: “Ponseti versus traditional methods of casting for idiopathic clubfoot.”
21. Morcuende J.A., Dolan L.A. et al.: “Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method.”
22. Zionts L.E., Ebramzadeh E. et al.: “Sixty Years On: Ponseti Method for Clubfoot Treatment Produces High Satisfaction Despite Inherent Tendency to Relapse.”
23. Sætersdal C. et al.: “Inferior results with unilateral compared with bilateral brace in Ponseti-treated clubfeet.”
PHOTOS & GRAPHICS:
1. Ni Hao Y’all
2. Clubfoot inside: Ponseti I.V.: “Congenital Clubfoot. Fundamentals of Treatment” (2nd edition)
3. Long-leg cast: Big Boy Story
4. Hoke tenotomy
5. Mitchell Boots and Brace and ADM
7. Scars after posteromedial release: Cure Organisation
8. Road image created by Rawpixel.com – Freepik.com
9. Other: own and supporting people of good will.