We know that the foot grows normally for the first several weeks in the pregnancy and then something happens that we don’t understand yet, and the foot twists.
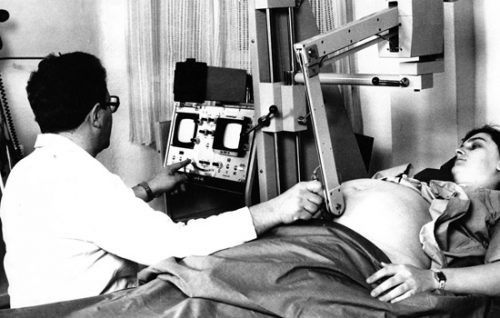
1958
First results of ultrasound imaging of clubfoot come from 63 years ago. 1958 was a key year for the first discoveries in this direction. Technological progress and the dynamically developing knowledge of the defect lead from timid attempts to describe the image seen to more and more bold analyzes. Over the years, ultrasound diagnostics has developed significantly, reducing the risk of an error. It does not change the fact that, many things cannot be perfectly explained and clarified and that this branch of medicine is still improving. Including the diagnosis of clubfoot.
HOW USS WORKS?
WHAT USS SHOWS?

WHEN?
Congenital clubfoot develops after 12 weeks of pregnancy, so it is difficult to see the defect earlier. What’s more – it may not be visible at all, even in the later stages of pregnancy. Most often, however, it is diagnosed between 16 and 23 weeks of gestation. Most of the defects are detected between 18 and 22 weeks of pregnancy. The knowledge, skills and experience of the doctor performing the examination and the quality of the equipment (the sensitivity of the probes is very important) are of great importance in detecting it, which allows not only simple imaging, but also the possibility of 3D and 4D imaging. The gestational age also affects the result. Transvaginal ultrasound gives better diagnostic results in the earlier weeks of pregnancy (14-16 weeks of pregnancy), and transabdominal ultrasound gives better results after 16 weeks of pregnancy.
EXPERIENCE

Regardless of which type of examination you choose – 2D, 3D, 4D – you must be aware that not every doctor can handle the diagnosis. Each gynecologist performs a basic examination (preliminary anatomical assessment of the basic elements), but good prenatal diagnostics requires an experienced doctor who specializes in this type of diagnosis. It happens that ultrasound examination in the field of gynecology is performed by radiologists, and if everything is fine and the pregnancy proceeds smoothly, it is not a major problem, but it should definitely be performed by a gynecologist specializing in radiology. It should also be remembered that even an experienced doctor may not notice a defect during the examination. You cannot blame him for “not seeing”, because correct diagnosis depends not only on his skills and equipment, but also on the positioning of the child, which cannot be turned so easily. .
WHAT IS ''A MID-PREGNANCY ULTRASOUND"?
TWO, THREE, FOUR
In general, clubfoot can be diagnosed during a routine 2D examination. If it is suspected that your child may have a defect, using 3D (three-dimensional) or even 4D (four-dimensional) imaging will undoubtedly be an advantage (not a necessary condition for diagnosis, but highly helpful). During 3D (three-dimensional) ultrasound, the child is visible on the monitor screen as a three-dimensional (placed in space), stationary body. Thanks to the three dimensions, it is much easier for a doctor to see the fetus from the outside, and therefore the feet can also be viewed, measured, if possible (depending on the child’s position). 4D (four-dimensional) ultrasound allows you to see a child in motion in a specific three-dimensional space, dynamically, which may translate into an even better diagnosis of the defect. Clubfoot is clearly visible during movement and in most cases leaves no illusions.
ULTIMATELY!
The increasing possibilities of equipment and advanced research into prenatal diagnostics enable a more accurate diagnosis of the defect. 60% of clubfoot are diagnosed during USS. Thanks to the scales. that are developed by doctors around the world, it is possible to determine the type of feet: typical and atypical, the degree of deformation and prognosis for further treatment, especially when clubfoot is the result of other, much more serious defects. However, all of this is under development and is not widely accepted. It also has many limitations. The prenatal diagnosis of clubfoot continues to struggle with many questions that doctors are looking for answers and solutions to. The conclusion is that diagnosis will finally be confirmed only after delivery. This means that on the basis of ultrasound examination, the doctor is not able to determine whether the feet are actually clubfoot or whether it is a positional defect, whether they are “standard” or atypical. It is also difficult to correlate the “degree” of the defect diagnosed during ultrasound with the actual image after delivery, because it is often not determined and recorded.
MISTAKE?

Despite more and more sensitive diagnostic probes, better and better ultrasound machines, and more and more advances in medicine and imaging diagnostics, many cases among diagnosed children do not have clubfoot in the end. Some studies say that the risk of detecting a “false-positive” (FP) is up to 30%, which is a high percentage. This is because the study does not exactly distinguish the type of defect between a true clubfoot that requires treatment and a POSITIONAL CLUBFOOT, which does not require or requires treatment, but is very “limited”. Attempts are being made to develop a scale that would allow a more accurate diagnosis of the foot type and the severity of deformation, but these attempts still face limitations. The risk of error is also related to the gestational age of the fetus during the examination, the quality of the equipment, the adopted methodology or the skills of the doctor-diagnostician: correct “reading” of the image and the ability to accurately perform measurements is important and not everyone has this skill. Also, the distinction between idiopathic defect, isolated defect, and atypical foot is very important, as the latter type of foot may be associated with other severe and lifelong disabilities or early death. Therefore, it is also important to inform parents during the diagnosis about the limitations of prenatal diagnosis.
SOMETHING MORE?
Congenital clubfoot is often a RESULT or companion of other defects and syndromes. Thus, if a foot defect is detected in the examination, it is the doctor’s duty to examine the child carefully and take more precise measurements of the relevant parameters. Of course, they are not always reliable. If it turns out that clubfoot is the result of something more serious, e.g. Down’s syndrome, it is advisable to do some additional tests, e.g. PAPP test, NIFTY test, karyotype or amniocentesis. A detailed family history is also the basis for a good diagnosis of any defects. Some of these tests are invasive and carry a risk of miscarriage – be aware of this. In most cases, the defect is idiopathic, which means that the cause is unknown. In this case, performing additional tests is not necessary and even debatable.
AMNIOCENTESIS
Some doctors believe that having an amniocentesis gives a partial answer confirming that the defect exists. However, when viewed realistically through the research, it does not contribute much when it comes to idiopathic clubfoot. An amniocentesis is an invasive test in which you take a sample of the amniotic fluid and test it. It is justified when there is a risk of other defects, because non-invasive prenatal examinations (e.g. the ultrasound scan between 11 and 14 weeks of pregnancy did not show the nasal bone of the child or the nuchal translucency index was very high) indicated the possibility of the occurrence of birth defects. The risk associated with amniocentesis is miscarriage, but – here is a paradox- the risk is also the formation of clubfoot with neurological background, when as a result od collecting the sample, the anterior peroneal nerve of the child was paralyzed (the test needle stuck in the front part of the shin), resulting in paralysis and deformity of the foot.
KARYOTYPE EXAMINATION
A karyotype is the complete set of chromosomes found in every cell in the body that has a nucleus. Each such cell (with the exception of reproductive cells) contains a set of 46 paired chromosomes. The karyotype test is performed on the basis of the patient’s blood sample, and its evaluation is made during the cytogenetic test. The sample is tested by analyzing genetic material from one of the lymphocyte (white blood cell) populations, but it can also be performed by analyzing cells derived from amniotic fluid (obtained through amniocentesis) or from tumor cells. Regardless of the type of material obtained from the patient, cells are grown in vitro. During the test, not only the number of chromosomes is assessed, but also their location and shape. Karyotype testing is not routine. For the examination by the mother, specific indications are necessary:
- previous experience of miscarriage (including recurrent miscarriages);
- the occurrence of miscarriages among close relatives of parents;
- previous deliveries of a stillbirth;
- already having a child with genetic defects related to chromosomal disorders.
There are indications for the examination of the fetus:
- abnormal results of non-invasive prenatal tests;
- the age of the mother over 35;
- diagnosis of chromosomal disorders in the child’s parents;
- the presence of genetic defects (related to chromosomal disorders) in the previous pregnancies of a given couple.
MAGNETIC RESONANCE IMAGING
The defect can be diagnosed more accurately by performing MRI or magnetic resonance imaging. It is not indispensable due to the strong radiation which is not insignificant for the mother and child and is not well understood. Performing magnetic resonance imaging as a routine examination, while no other abnormalities have been found in ultrasound, is highly debatable mainly because of its yet unknown effects on the fetus and the mother .
DISPUTES
There are discussions between clinicians about the necessity of performing MRI, amniocentesis and karyotyping during the diagnosis of idiopathic clubfoot.
Some of them believe that, for example, the karyotype test is necessary, due to the possibility of finding other damaged genes that indicate a possible combination of the defect with other, more advanced defects.
Some of them believe that studying the karyotype is not of great importance, as in most cases there are changes in individual genes anyway. Some studies say that the performance of this test in mothers and children who had the defect did not provide important information for diagnosis.
RELABILITY
Prenatal diagnosis of clubfoot is helpful in postnatal treatment planning but should be as accurate as possible: misdiagnosis can cause excessive stress to parents and can lead to unnecessary invasive testing. Conversely, well-performed diagnosis can ease parental anxiety, rule out invasive testing, and help parents understand the defect and prepare for better treatment. The ability to properly advise patients requires a physician to carefully diagnose both the deformity of the foot itself and any other related abnormalities.
IF YOU ALREADY KNOW THAT YOUR CHILD CAN HAVE CONGENTIAL CLUBFOOT, SET THE DIRECTION OF YOUR ACTION.
GET THE KNOWLEDGE YOU NEED: BEGINNING WHAT THE DEFECT IS, THROUGH ITS TREATMENT, UP TO INFORMATION ABOUT POTENTIAL DIFFICULTIES RESULTING FROM THE SPECIFICITY OF THIS DEFECT.
YOU CAN ALSO CONTACT A DOCTOR WHO HAS EXPERIENCE IN DIAGNOSING AND TREATING THIS DISEASE.
ESTABLISH A TREATMENT STRAGEGY WITH THEM, SO THAT AFTER BABY IS BORN,
YOU CAN MAKE THE MOST OF THE TIME TO BE WITH YOUR CHILD AND JOY THAT HE IS ALREADY NEARBY.
SOURCES
RESEARCHES & STUDIES:
1. How does the USS works?
2. Bar-On E., Mashiach R. et al.: “Prenatal ultrasound diagnosis of club foot: outcome and recommendations for counselling and follow-up.”
3. Faldini C., Fenga D. et al.: “Prenatal Diagnosis of Clubfoot: A Review of Current Available Methodology.”
4. Glotzbecker M.P et al.: “Prenatally diagnosed clubfeet: comparing ultrasonographic severity with objective clinical outcomes.”
5. Mahan S.T., Yazdy M.M. et al.: “Prenatal screening for clubfoot: what factors predict prenatal detection?”
6. Radler C., Herzenberg J. E. et al.: “Maternal attitudes towards prenatal diagnosis of idiopathic clubfoot.”
7. Nemec U., Nemec S.F. et al.: “Clubfeet and associated abnormalities on fetal magnetic resonance imaging.”
PHOTOS & GRAPHICS:
1. USS probes
2. USS
3. Doctor experience
4. Medical photo created by rawpixel.com – www.freepik.com
5. Support group for parents
6. Other: own and thanks to people of good will





